We use cookies
We use cookies to ensure that we give you the best experience on our website. Would you like to accept all cookies for this site?
Bikkel, Uroabdomen and Cystorrhexis
Introduction
Bikkel presented to our WVS clinic in Ooty with a history of falling from a height. A diagnostic work up found that Bikkel's urinary bladder has ruptured and he had urine free-flowing into his abdomen. Our vets worked quickly to stablilise Bikkel so that they could perform surgery to fix his bladder. Here is his story.
History
Bikkel, a Belgian Malonois dog presented to our clinic with a history of falling, a distended abdomen, vomiting, dehydration, laboured breathing and he had not passed urine for 3 days.
Signalment and Clinical Signs
A male, intact, Belgian Malinois dog, weighing 39 kg and approximately 6 years old. Deworming and vaccination status was up-to-date.
Physical examination
The dog was dull but responsive. Physical examination revealed a distended abdomen with a fluid thrill. Pain on abdominal palpation was evident. Temperature 37 degC (mild hypothermia), heart rate 64 bpm, respiratory rate 36 bpm with dyspnoea, CRT 2 secs, estimated at 5-7% dehydrated, peripheral lymph nodes NAD. and hypothermia were noticed.
Differential Diagnosis
Based on the clinical findings, the following list of possible diagnoses were considered:
- Ascites
- Uroabdomen
- Haemoabdomen
- Peritonitis
- Neoplasia
Diagnostic Work Up
Abdominocentesis
Abdominal palpation revealed a distended abdomen with a fluid thrill, indicating the presence of free fluid. Abdominocentesis was performed using a 20 G x 1.5” needle in order to characterise the type of fluid present (Fig 1).
Bikkel was placed in left lateral recumbency. A 10 x 10-cm area was clipped and aseptically scrubbed along the ventral midline. The needle was inserted caudal to umbilicus, 2 cm right of midline, with the needle pointing caudally towards the pelvis. The fluid removed is shown in Figure 1.

Figure 1 - Image of the fluid taken from Bikkel's abdomen during abdominocentesis
The laboratory results of the peritoneal fluid are given below:
| Parameter | Result | Parameter | Result |
|---|---|---|---|
| Colour | Reddish | Ketones | Negative |
| Appearance | Slightly cloudy | RBCs | >100 RBC/HPF |
| Specific Gravity | 1.020 | Leucocytes | 5-25 WBC/HPF |
| pH | 7.0 | Crystals | Nil |
| Protein | 300 mg/dl | Glucose | Negative |
| Epithelial cells | Few transitional epithelial cells |
Key indicators of a uroabdomen would be high creatinine levels (2-4 x) in the abdominal fluid compared to serum; potassium levels are also higher in the peritoneal fluid. Waste products (urea) and electrolytes such as potassium are reabsorbed over time, resulting in an azotaemia and hyperkalaemia, which must be addressed as can be life threatening. Due to its large molecular size, creatinine is not reabsorbed and levels remain high in the leaked fluid compared to those in the blood.
Plain Radiography
Lateral abdominal radiographs revealed a fluid filled abdomen. Note the lack of abdominal detail. (Fig 2).

Figure 2 - Plain radiograph of Bikkel's abdomen showing an absence of definition of the addominal organs consistent with a fluid-filled abdomen
Haematology and Serum Biochemistry
Haematology revealed leucocytosis with neutrophilia; other parameters were in normal range.
| Parameter | Result | Reference range |
|---|---|---|
| WBC | 22 x 10^3/Cu.mm | 6.0 – 17.0 10^3/Cu.mm |
| Neutrophils | 80% | 62-77% |
Serum biochemistry showed a marked increase in creatinine and BUN (Blood Urea Nitrogen) levels (azotaemia). A marked hyperkalaemia was also seen. Serum sodium and chloride levels were below the normal limits.
| Parameter | Result | Reference range |
|---|---|---|
| Creatinine | 11.98 mg/dl | 0.5 – 1.5 mg/dl |
| BUN | 212.3 mg/dl | 10.0 – 28.0 mg/dl |
| Sodium | 122.1 mmol/L | 141 – 152 mmol/L |
| Potassium | 7.9 mmol/L | 4.37 – 5.35 mmol/L |
| Chloride | 89.0 mmol/L | 105 – 115 mmol/L |
Definitive Diagnosis
Uroperitoneum/uroabdomen associated with the rupture of urinary bladder (cystorrhexis).
Treatment Plan
Aggressive emergency fluid therapy to stabilise the patient and to correct electrolyte and metabolic imbalances is essential before undergoing surgery to correct the ruptured bladder.
Initial therapy
It is important to address the water and electrolyte imbalances prior to starting surgery to reduce the anaesthetic risk for the patient. In this case, this was achieved with lactated Ringer's solution for rehydration, and 10% calcium gluconate @0.5 mL/kg slow IV as a cardio-protectant due to the high potassium levels. In addition, the following were administered:
- Ranitidine @ 2mg/kg IV TID (as a gastro-protectant against uraemic gastritis)
- Amoxicillin-clavulanate @ 20 mg/kg IV BID
- Buprenorphine @ 0.05 mg/kg IV once every 6 hours
The surgical procedure
The following protocol was used for premedication and anaesthesia.
Premedication Diazepam (0.25 mg/kg) slow IV + buprenorphine (0.05 mg/kg) intramuscularly.
Induction Propofol (1mg/kg) slow IV.
Pre-op antibiotic Amoxicillin-cloxacillin (20mg/kg) IV.
After induction, Bikkel was intubated with an endo-tracheal tube to stabilise his airway and provide emergency access.
Anaesthesia maintenance General anaesthesia was maintained under Isoflurane (2%).
Bikkel was positioned in dorsal recumbency, the surgical site was clipped and scrubbed with chlorhexidine followed by isopropyl alcohol spray.
A linear incision was made from umbilicus to pubis, through the skin. The subcutaneous tissue was bluntly separated, and the abdominal musculature and peritoneum were incised via the linea alba. Reddish coloured fluid (urine) started gushing out from the surgical wound when the abdominal cavity was entered. This was fully removed using suction.
The urinary bladder was located and exteriorised with large gauze swabs placed underneath and either side of it to keep it exteriorised. This allowed the surgeon to evaluate the extent of the rupture; blood clots had formed at the end of torn vessels so it wasn’t actively bleeding at this point (Fig 3).
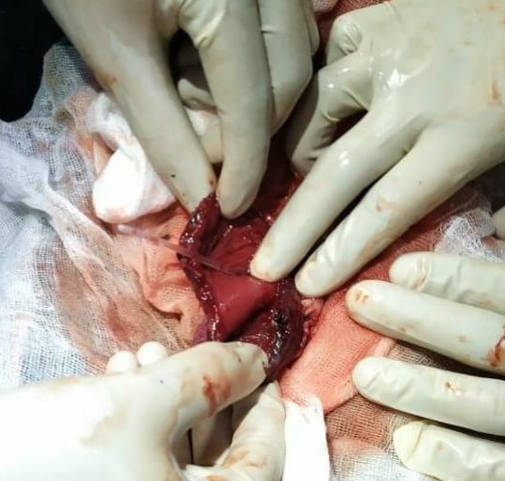
Figure 3 - Ruptured bladder as seen when exteriorised during surgery
The edges where the bladder had ruptured were freshened by trimming the edges with mayo scissors. This ensures that when sutured together, the edges have a fresh blood supply to encourage healing.
The bladder was closed (cystorrhaphy) with a two-layer inverting suture pattern using 2-0 polydioxanone (PDS) (Fig 4). The peritoneal cavity was then lavaged extensively with large volumes of body-temperature saline.
An indwelling urethral catheter was left in place for decompression. The abdominal muscles, subcutaneous tissue was closed in simple continuous pattern using polyglycolic acid (PGA)1-0 and skin was closed with polyamide 2-0 and an interrupted cruciate pattern.

Figure 4 - The bladder was closed using a two-layer inverting suture pattern
Post-Operative Care
Post-operatively, Bikkel continued to receive fluid therapy, systemic antibiotics and analgesics.
-
Analgesics
- Buprenorphine @ 0.05 mg/kg IV every 6 hours for 5 days
- Meloxicam @ 0.1 mg/kg SC was given from the second day for 3 days
-
Antibiotics
- Amoxicillin - clavulanate (20 mg/kg) IV BID
- Metronidazole (10mg/kg) IV BID for 7 days
- Ranitidine @ 2mg/kg IV TID for 5 days
An Elizabethan collar was used to prevent Bikkel from biting or licking his surgical site. Strict rest and short leash walks were recommended for 2 weeks.
Bikkel recovered uneventfully without any complications. Within 5 days of surgery, haematology and serum biochemistry values returned to normal range. The indwelling urethral catheter was left in place for 48 hours after the surgery for decompression. The skin sutures were removed on the 7th day.

Figure 5 - Bikkel and his owner at his final post-op check after a full recovery
Discussion
Damage to the urinary bladder is a common consequence of large trauma in small animal practice. Patients with a ruptured bladder often do not show clinical signs immediately after injury. However, they become dehydrated and develop severe electrolyte and metabolic disturbances over the subsequent 24 to 48 hours. Blunt abdominal trauma is the most common cause of bladder rupture in dogs and cats.
The most common clinical signs are abdominal pain and distention, anorexia, dehydration, lethargy and hypothermia. Azotaemia, hyperkalaemia, metabolic acidosis and an elevated neutrophil count are the commonly reported laboratory findings.
When urine leaks into the abdominal cavity, some nitrogenous waste products and electrolytes are reabsorbed across the peritoneal membrane and re-enter the circulation. Urea rapidly equilibrates across the peritoneal surface, whereas creatinine cannot pass back into blood stream and remains concentrated in the abdominal fluid. Comparisons of creatinine and potassium concentrations in peritoneal fluid and serum are the most reliable tests for confirming uroabdomen in dogs and cats. Reported mean ratios of abdominal fluid : serum creatinine concentrations in case of uroabdomen are 5:1 in dogs and 2:1 in cats; reported mean ratios of abdominal fluid : serum potassium concentrations are 2.5:1 in dogs and 1.9:1 in cats.
In the plain abdominal radiographs, the loss of abdominal details caused by fluid accumulation was marked. Alternative methods to establish bladder rupture could be:
- Positive-contrast urethrocystography
- Ultrasonographic examination should detect fluid accumulation in peritoneal space and can be used to guide abdominocentesis.
- Surgical exploration of the abdominal cavity (exploratory laparotomy) plays an important role in diagnosing uroabdomen, especially in situations in which fluid analysis has confirmed urine leakage and imaging studies couldn’t verify the site of leakage.
The goal of initial treatment is to stabilise the patient for surgery. Principle areas of concern are azotaemia, electrolyte and acid-base disorders, and cardiac arrhythmias caused by severe hyperkalaemia. Drainage of urine from the abdomen is the second most important step. This can be achieved through placement of a peritoneal lavage catheter or at exploratory surgery if the patient is rapidly stabilised.
Hyperkalaemia causes bradycardia, flattened P wave, prolonged P-R intervals, widened QRS complexes, tented T waves, in addition to predisposing to cardiac arrhythmias. Potassium concentrations greater than 7 mEq/L may cause irregular idioventricular rhythms, and potassium concentrations exceeding 9 mEq/L commonly cause atrial standstill. Historically, 0.9% saline was recommended because of its lack of potassium; however, lactated Ringer’s solution may be as effective as 0.9% saline in reducing potassium concentrations and more efficient in normalising acid-base status and other electrolytes.
Hyperkalaemia from uroabdomen responds well to abdominal drainage plus intravenous fluid therapy. If hyperkalaemia is life threatening, 10% calcium gluconate (0.2-1.5 ml/kg) can be given for transient cardiac protection. Give slowly (over 5-10 minutes) whilst monitoring the patient’s ECG. Resolution of urine retention is critical for normalising electrolytes and acid-base status and resolving azotaemia.
Bladder rupture generally occurs near the apex. Surgical exploration and repair are indicated in most cases. If the bladder is notably thickened, single-layer anastomosis pattern is performed; otherwise, a two-layer inverting pattern. Absorbable suture materials like polydioxanone (PDS) or poliglecaprone 25 (Monocryl) are preferred for bladder and urethral surgery.
Post surgery, intravenous fluids should be given until the animal is able to drink adequate fluids to maintain hydration. If bladder atony is present, the bladder should be kept decompressed by intermittent urinary catheterization or by manual expression once the bladder has healed. An α-blocker (e.g., phenoxybenzamine) and/or a somatic muscle relaxant (e.g., diazepam) can help decrease urethral sphincter tone. Bethanechol is a cholinergic that increases detrusor contractility and may aid voiding.
The major complication of bladder surgery is urinary leakage, especially if a watertight seal is not achieved or if devitalized tissues are sutured and subsequently dehisce. Occasionally, peritonitis may occur from infected urine or secondary to surgically induced contamination.
The prognosis is excellent for animals with traumatic bladder rupture. Occasionally, rupture secondary to obstruction may have a guarded prognosis if the majority of the bladder is necrotic.
Conclusion
Exploratory surgery was performed to resolve uroabdomen and cystorrhaphy to correct the ruptured bladder. Bikkel made an uneventful recovery. The surgical experience and preparedness of the WVS ITC team was of paramount importance in the successful outcome of this case.
References
- Fossum, T. W. (2013). Small Animal Surgery, 4 Elsevier Mosby. 3251 Riverport Lane St. Louis, Missouri. pp 735-759.
- Grayson Cole and Karen M. Tobias (2013). Emergency Urinary Bladder Surgery. Clinician’s brief, November 2013 Edition, 35-39.
- Phillip Mayhew and David Holt (2004). Ruptured Bladder in Dogs and Cats. Standards of Care Emergency and Critical Care Medicine, November 2004, Volume 6.10. pp 1-6.
- Schmeidt C, Tobias K, Otto C. Evaluation of abdominal fluid: peripheral blood creatinine and potassium ratios for diagnosis of uroperitoneum in dogs. J Vet Emerg Crit Care. 2001;11(4):275–280.

About the author
Dr. Sumanth Bedre is one of our senior vets at WVS ITC in Ooty, India and has been working with WVS since October 2020. He graduated with Bachelor’s in Veterinary Science and Animal Husbandry (B.V.Sc & A.H) in 2016 and completed his Masters in Veterinary Pathology (M.V.Sc) in 2018. He is very much interested in emergency and critical care, he is actively involved in ITC activities and outreach projects.
© WVS Academy 2026 - All rights reserved.