We use cookies
We use cookies to ensure that we give you the best experience on our website. Would you like to accept all cookies for this site?
Coffee, Gastric Foreign Body
Introduction
What a lucky puppy! Coffee had a gastrointestinal foreign body that was treated at the WVS Rescue and Rehabilitation Centre in Thailand. Coffee, who lives in a military camp in a Northern Subdistrict of Chiang Mai, Chiang Dao, ate whole a grilled pork kebab-style snack including the 10cm long sharp stick! The stick pierced his stomach and luckily he was brought quickly to our vet team to perform emergency surgery before the stick could do further damage. Here is his story.
History
Coffee, a community puppy from a military camp in Chiang Dao, came to WVS Thailand with a prominent, firm, foreign body which was visibly distending his abdominal wall outwards just behind his last rib. The caretakers who brought Coffee in said that they gave him a grilled pork kebab which he then ate whole, including the sharp stick. This incident happened one day before Coffee's caretakers brought him to WVS Thailand for an assessment and treatment.

Signalment and Clinical Signs
Coffee was a mixed-breed male dog, 5 months old with gentle behaviour. His weight was only 5.5 kg when he came to WVS Thailand and he had no history of vaccination or parasite treatment.
Clinical findings at presentation to WVS Thailand
- Bright, alert and responsive.
- Defecating, urinating, drinking, eating normally. No vomiting or diarrhoea.
- Cardiovascular: Heart sound was normal, strong femoral pulse, pink mucous membranes, capillary refill time < 2 secs, normal hydration.
- Body temperature: 39.4°C (possibly due to the long car journey to the clinic).
- Respiratory: normal lung sounds and normal respiratory patterns.
- Skin: normal hair coat, nothing significant found.
- Body condition score: 3/5.
- Musculoskeletal: Nothing significant found.
- Reproductive: Nothing significant found.
- Abdomen: Prominent part of the stick palpated just behind the last rib, pain elicited when we changed the position of the dog (Figures 1 and 2).
- Eyes, Ears, Nose, Throat: Nothing significant found.

Figure 1 — Protrusion from body surface due to the presence of a large, foreign body (arrow)

Figure 2 — Another area of protrusion in a ventral position (arrow)
Differential diagnosis
Gastrointestinal foreign body: The foreign body might be in the stomach or intestine, so we took a radiograph and performed ultrasound to help narrow down the location.
- Gastric foreign body
- Intestinal foreign body
Diagnostic work up
Radiography
2 orthogonal views were taken. It was not possible to see the stick clearly here as the stick is a similar opacity to soft tissue (Figures 3 and 4). Abnormalities were not seen.

Figure 3 — Left lateral radiograph

Figure 4 — Ventro-dorsal abdominal radiograph
Ultrasonography
There was an acoustic shadow cast by the stick in the area of the stomach (Figure 5).
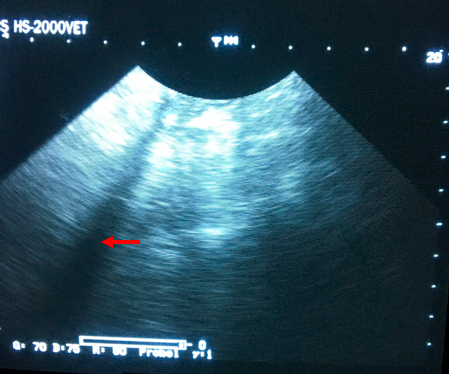
Figure 5 — Ultrasound image at the location of the stick. Note the long, thin shadow cast by the foreign object.
The radiography and ultrasound did not conclusively locate the stick, but we knew from palpation that it was in the upper abdominal area.
Treatment
A normal sedation and anaesthesia preparation protocol was used and anaesthesia was maintained using isoflurane.
Laparotomy: A standard ventral midline incision was made. We found the large stick in the stomach; the sharp end of the stick had penetrated through fundus of the stomach (Figures 6 and 7) and the abdominal wall, and was lodged in the subcutaneous layer on the back of the patient. No other internal organs were damaged.
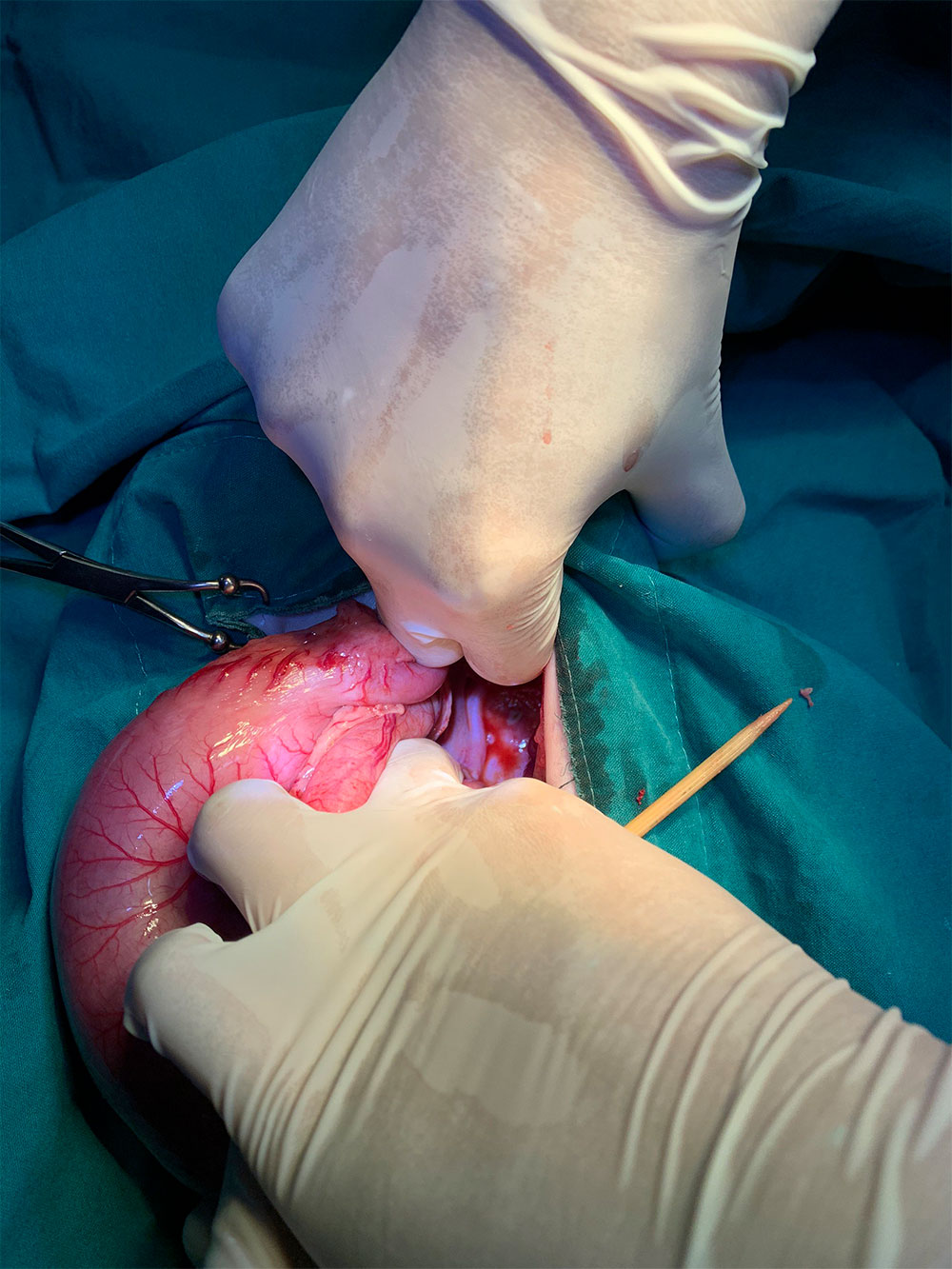
Figures 6 & 7 — Images showing the serosal surface of the stomach with focal lesions caused by penetration by the sharp end of the stick.
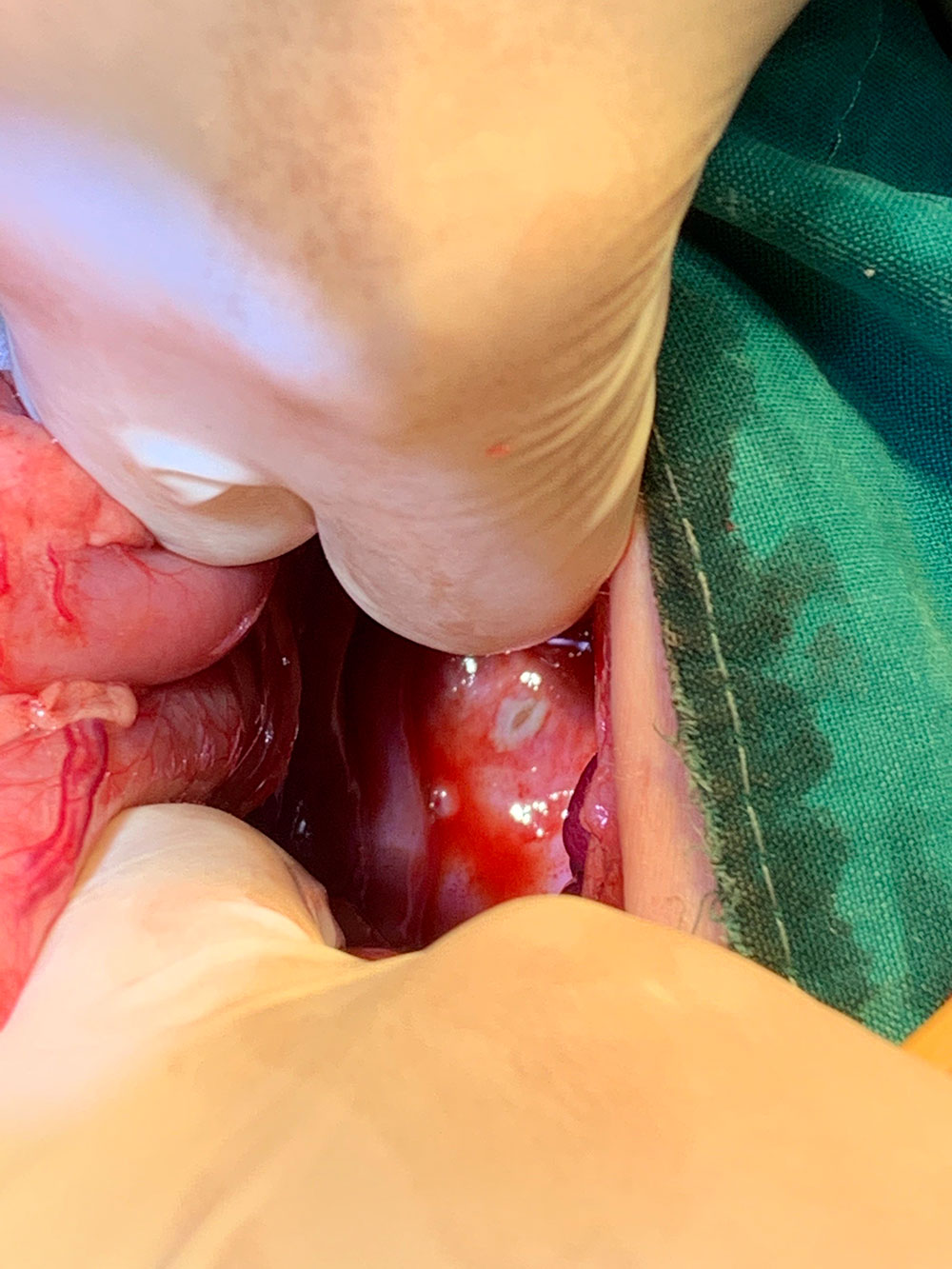
Gastrotomy: To begin with, a stay suture was placed through the serous layer of the stomach to ensure it did not slip back into the abdomen (Figures 8 and 9).

Figures 8 & 9 — Placement of stay suture in the serous layer of the stomach
The stick was then removed from the stomach via the hole that it had created near the fundus region (Figure 10).

Figure 10 — The sharp stick that was removed from Coffee's stomach
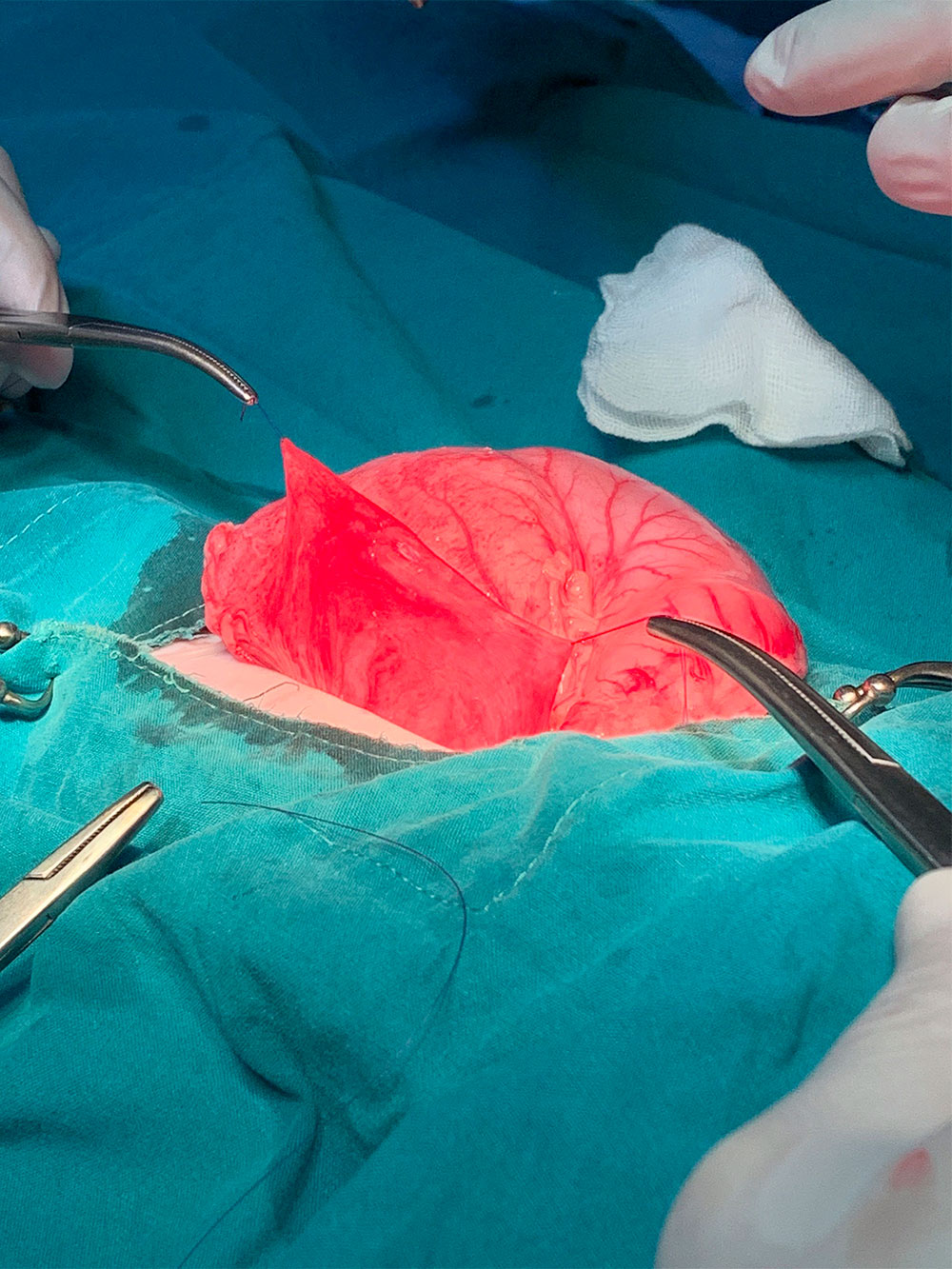
The necrotic tissue was then debrided from around the opening in the stomach. Once all dead tissue was removed, the gastrotomy hole was closed with monocryl 4/0 using a continuous subcuticular pattern for the inner layer and an inverting pattern for the outer layer (Figure 11).
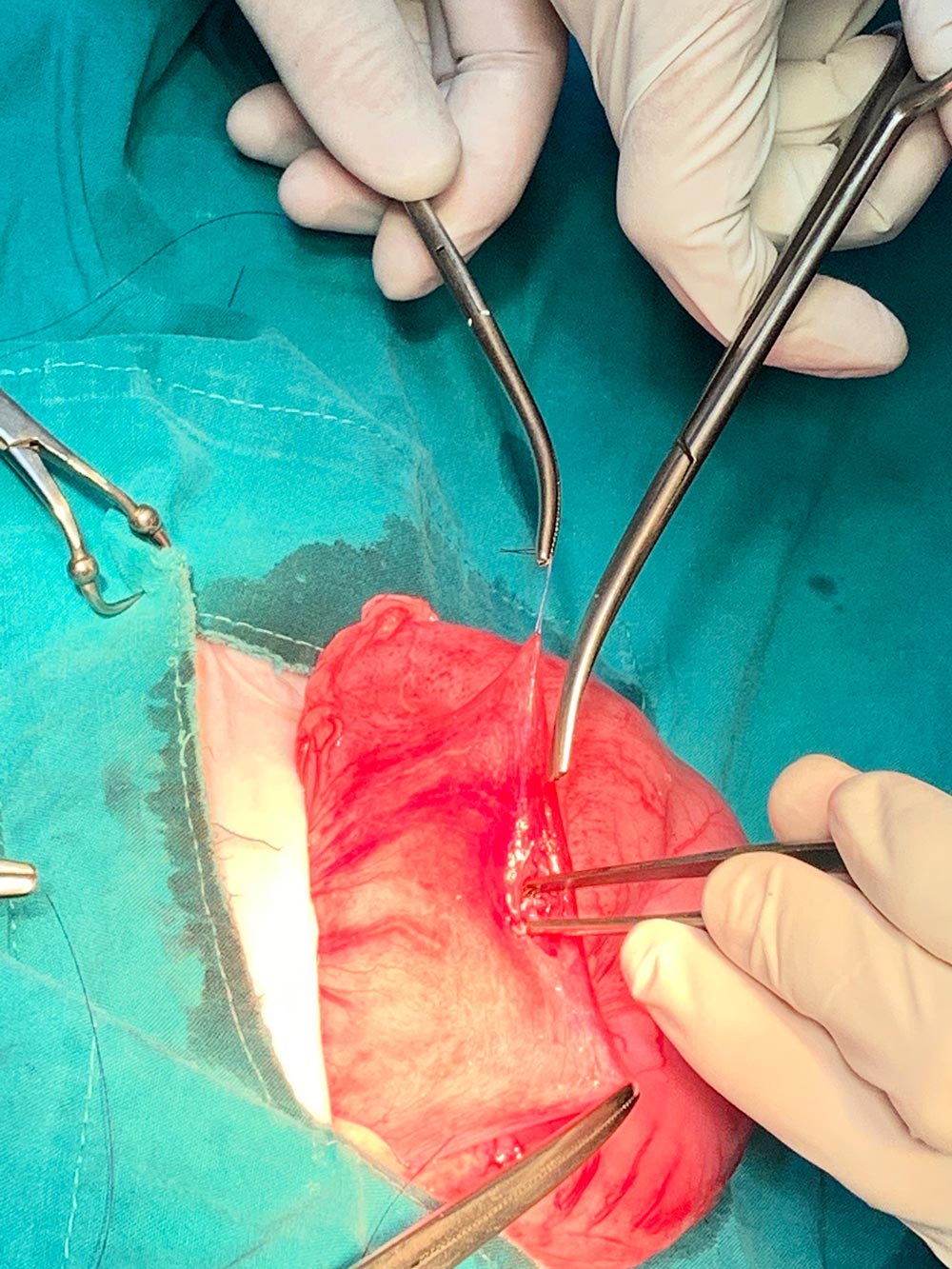
Figure 11 — Closure of the stomach wall using a continuous subcuticular pattern for inner layer and an inverting pattern for the outer layer by using monocryl 4/0.
Once these 2 layers were completed, the integrity of the stomach wall was assessed. The surgeons determined that a small amount of gastric contents could still leak through and so added an additional inverting suture layer. The omentum, which is an excellent source of blood vessels and can help fill in the gaps between the sutures of an abdominal surgery, was sutured lightly across the gastrotomy site using a simple interrupted pattern.
Then, the muscle layer was closed with PGA 0 by using a simple continuous pattern with 6 knots along the surgical wound, then the subcutaneous layer using PGA 2/0 with subcutaneous continuous pattern and the skin using an intradermal (buried) suture pattern.
Post-operative care
For his post-operative pain relief and prophylactic antibiotic treatment, Coffee received:
- Meloxicam 0.2mg/kg once per day by mouth for 5 days
- AMC syrup 20mg/kg twice per day by mouth for 7 days
Coffee was closely monitored for abnormalities such as depression, vomiting, diarrhoea and loss of appetite after his op and his exercise was limited to a few short toileting walks per day to begin with. His incision site was checked daily for signs of discharge and hernia, and she was fed a bland diet split into small frequent meals.


Figures 12 & 13 — Images of the surgical wound after surgery at day 1 (left) and day 7 (right) showing the surgical was completely healed without complication.
Prognosis
A gastric foreign body prognosis generally depends on:
- the location of the foreign body
- the size, shape, and characteristics of the foreign body
- the health status of the pet before the foreign body was ingested
- if the foreign body caused an obstruction, and the duration of the obstruction
If the surgery is uncomplicated and a perforation doesn't occur, the prognosis is considered excellent. If a perforation does occur and causes peritonitis, then the prognosis depends on the severity of the peritonitis and the combination of the above factors.
In this case, whilst a perforation did occur, gastric contents did not spill into the abdomen and cause a peritonitis because the perforation was kept plugged by the stick itself. After removal of the stick, Coffee's prognosis was excellent.
Coffee's appetite remained good with increased alertness compared to prior to admission. There were no signs of inflammation, irritation or swelling of the surgical site. She was eventually discharged.
Discussion
Foreign body ingestion is relatively common in dogs. They tend to be curious and greedy and this can occasionally get them into trouble. Sometimes owners will see a dog ingesting a foreign object and other times they will notice the signs of a gastrointestinal foreign body without knowing the cause.
Clinical signs of a gastrointestinal foreign body are usually associated with pain or obstruction of the gastrointestinal tract. These include: loss of appetite, depression, vomiting, possibly diarrhoea or lack of faeces production. If an obstruction occurs or the ingested substance causes a perforation of the gastrointestinal tract occurs, this can lead to spilling of gastrointestinal contents into the abdomen causing a potentially fatal peritonitis. Further diagnostics and urgent medical and/or surgical care is required if a foreign body is suspected.
Diagnostics for a gastrointestinal foreign body include:
- patient history
- clinical signs
- palpation of the object in the abdomen
- ultrasonography
- radiography
- computed tomography (CT)
- exploratory laparotomy
Foreign bodies may be easy to observe using diagnostic imaging if their shapes are distinct and they are composed of substances that are more radio-opaque than soft tissue or fluid e.g. metal, bone, plastic. However, other foreign bodies are very difficult to see on x-ray or ultrasound as their opacity may be similar to that of the soft tissues surrounding them. In this case, clinicians will be looking for other signs that the intestines aren't working as they should be. For example, gas build up in the intestines (indicating an obstruction) or lack of definition of the abdominal organs (indicating a peritonitis). If a clinician is unsure about a foreign body presence, a contrast medium, e.g. a barium meal, could be used to observe the gastrointestinal tract by x-ray in more detail.
An exploratory laparotomy could be a valid diagnostic and, if a foreign body is found, it is a curative procedure. The patient's physical state and ability to manage anaesthesia should be made before deciding on this procedure as a diagnostic method, but ultimately if there is a foreign body, it will need to be removed by this method either way.
The history which was taken from Coffee's caretakers gave our veterinary team a pretty clear indication that he had a gastrointestinal foreign body. This was confirmed through palpation of the stick within Coffee's abdomen. We were not sure where the foreign body was located exactly so we decided to conduct additional diagnostic imaging with radiography and ultrasonography. This didn't give us an exact location beyond caudal abdomen, and so we opted to continue with the exploratory laparotomy and foreign body removal.
After that, we found the large shape stick located in the stomach and the sharp end of the stick penetrates through the stomach irritating abdominal wall. Fortunately, we did not find other internal organs damaged, nor found any complication after surgery and he had recovered as well. The blood test should be performed before surgery, but we have enough time to wait for blood result because this condition was an emergency situation, there often is not time for many diagnostic measures and surgery may be attempted as soon as possible. The next time, if we have time, we should perform blood test before surgery and the blood test can help us rule out some conditions in diagnosis.
A foreign body located in the stomach can sometimes be removed with non-surgical endoscopy if it is small enough. However, if the foreign body is sharp or too large, it may not be able to be safely removed this way. The longer the foreign body is stuck within the GI tract, the worse the damage to the GI tract often is. Surgically opening the stomach or intestines is often performed, but sometimes, a damaged section of gastrointestinal tract needs to be removed.
The overall risk of this surgery is low. The major risks are those of general anaesthesia, bleeding, postoperative infection and wound breakdown over the incision. Other complications maybe be dependent on the underlying cause of the surgery as well as other concurrent diseases. Overall complication rate is low.
Post operative care is very important. The patient should be closely monitored for depression, vomiting, diarrhoea or loss of appetite, as this may indicate presence of intestinal or stomach leakage. If this occurs it is most likely in the 3–5 days postoperatively. As Coffee is a community dog, our veterinary team decided to keep Coffee at the Rescue and Rehabilitation centre until his wound completely healed and all treatments were finished.
Pain medication and antibiotics may be given as needed. The pain medication that we choose was meloxicam, which is a non-steroidal anti-inflammatory drug (NSAID) used to relieve pain, inflammation, and fever in dogs. Meloxicam is also used to treat pain associated with surgery. Amoxicillin-clavulanic acid syrup was chosen because it is an antibiotic used to treat infections caused by gram-positive and gram-negative bacteria that might infect abdomen and gastrointestinal tract after surgery.
A bland diet in small, frequent meals was given to Coffee for two days after the procedure, with a gradual return to normal food. Coffee's activity was also limited to give his surgical wound the best chance to heal without complications.
Fortunately, Coffee's recovery went very well and he was returned to his caretakers 7 days after his surgery.
References
- Fossum, Theresa Welch (2007). Surgery of the stomach. Small animal surgery Third edition (pp.409 to 413). St.Louis, Mosby Elsevier
- Van Goethem, B. (2015) Gastro-Intestinal Foreign Bodies (Do's and Don'ts). World Small Animal Veterinary Association World Congress Proceedings. Available at:
https://www.vin.com/apputil/content/defaultadv1.aspx?id=7259318&pid=14365&
[Accessed 29 October 2021] - Hunter, T and Ward, E. Ingestion of Foreign Bodies in Dogs. Available at:
https://www2.zoetis.co.uk/products-solutions/dogs/gastrointestinal-foreign-bodies
[Accessed 28 October 2021] - Gastrointestinal foreign bodies in dogs and cats. Medivet. Available at:
https://www.medvetforpets.com/gastrointestinal-foreign-bodies-fb-dogs-cats
[Accessed 27 October 2021] - Tailwind Veterinary Surgery Care. Post-operative instructions. Available at:
http://www.vscdsurgerycenters.com/pdf/discharge-instructions/gastrotomy_discharge.pdf
[Accessed 27 October 2021]

About the author
Dr Pavanrut Vikan (AKA Kaotung) started working at WVS Thailand in January 2021. She was one of our Thai Surgical Students and enjoyed her time with us so much, once she graduated she asked for a job.
Dr Kaotung has a keen interest in surgery and has been developing her skills with our team. She is responsible for every day surgical and diagnostic duties in the Jeanne Marchig International Training Centre and Rescue and Rehabilitation Centre.
© WVS Academy 2026 - All rights reserved.