We use cookies
We use cookies to ensure that we give you the best experience on our website. Would you like to accept all cookies for this site?
Happy, Aural haematoma with concurrent Malassezia spp overgrowth
Introduction
Happy is one of the resident dogs at the WVS Thailand Rescue and Rehabilitation Centre. A volunteer noticed that her ear had become swollen and our vets identified that she had developed an aural haematoma. Happy underwent surgical draining of her ear and now receives regular check ups and ear cleaning to prevent reccurence of this problem. This is the story of her treatment.
History
Happy is 7 years 8 months old and weighs 28.3 kg. A volunteer dog walker noticed that her right ear was swollen and her caretakers had seen her scratching her ear and occasionally shaking her head.

Figure 1 — Happy in the sunshine!
Clinical signs
Happy's clinical exam did not reveal any abnormal clinical signs apart from her swollen right ear. The affected pinna was distended with fluid with significant amounts of dark brown, odorous, waxy discharge located within the ear canal and across the pinna. An examination of her tympanic membrane (ear drum) confirmed it was intact. Palpation of the affected pinna and ear canal elicited a pain response from Happy.

Figure 2 — Happy's ear before any treatment was given. Note the distended medial aspect of the pinna with signs of trauma to the skin.
Differential diagnosis
The causes of a fluid filled expansion of the pinna can be due to:
- Aural haematoma
- Pinnal abscess
- Cyst
- Neoplasia
In this case, an aural haematoma was considered the most likely diagnosis. However, this is not strictly a diagnosis, but a consequence of an underlying issue affecting the ear. Aural haematomas commonly develop as a result of physical injury to the ear pinna, such as scratching or head shaking, which results in the rupture of a blood vessel. Free blood accumulates under the skin, causing distention, inflammation, and pain. The reason why the patient is scratching or shaking its head must be identified. Otitis externa (inflammation of the external ear) can arise from the following primary and secondary disorders:
Primary:
- Hypersensitivity (atopy, food, contact)
- Parasites
- Foreign bodies
- Trauma (bite wound or blunt trauma)
- Neoplasia
- Endocrine disorders
- Conformational abnormalities
- Keratinisation disorders
- Juvenille cellulitis
- Inflammatory polyps
Secondary:
- Bacterial infection
- Yeast infection
- Otitis media
- Chronic pathological changes to the ear (e.g. chronic haematoma, ceruminous gland hyperplasia)
Once identified, it is important to address the underlying pathology, as well as the aural haematoma, in order to reduce the likelihood of recurrence. The vets working on this case suspected that the underlying cause was most likely to be irritation from infection and/or parasites due to the presence of the malodourous material in the external ear canal.
Diagnostic work up
A swab of Happy's ears was taken for cytology. The sample material was transferred to a microscope slide and stained using 'Diff-Quick'. The cytology result showed a significant overgrowth of Malassezia pachydermatis organisms in the affect ear canal, which were suspected to be the cause of the irritation and inflammation. Malassezia pachydermatis are characterised by their appearance under a microscope as little 'snowmen' with a small circle on top of a larger circle (Figure 3).
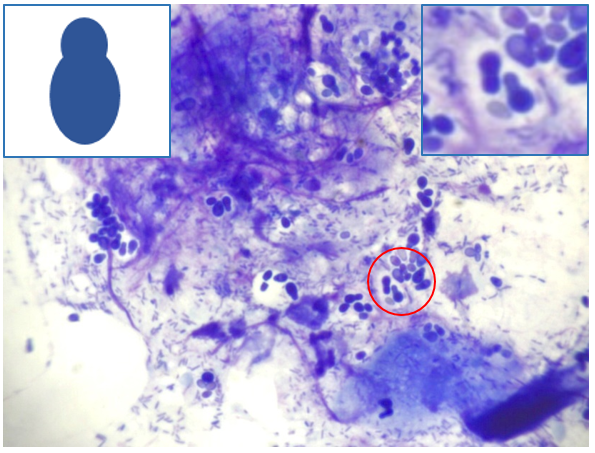
Figure 3 — Malassezia organisms are visible (circle), as well as numerous bacteria on this stained cytological smear of the ear canal. Inset, left: an illustration to show the shape of a Malassezia yeast. Inset, right: high power image of the stained Malassezia spp. Diff-Quik stain. x100 mag with oil objective.
Treatment protocol
Initially, the aural hematoma was managed medically by draining the subcutaneous blood using a large gauge needle and a 20 ml syringe. It is important to maintain sterile conditions by cleaning the skin with antiseptic solution beforehand and wearing clean gloves, in order to prevent introducing infection. Once the fluid was drained, a bandage was used to apply mild pressure on the pinna, to discourage further bleeding. Unfortunately, the haematoma had reappeared the next day. At this point, a surgical intervention was required.
The patient was anaesthetised and the ear aseptically prepped for surgery. An incision was created down the length of the concave (medial) aspect of the pinna (Figure 4). (An 'S' shaped incision can be made as an alternative). Fluid and blood clots were removed completely. To discourage the subcutaneous tissues from refilling with fluid, several vertical sutures were placed either side of the surgical wound on the medial aspect of the ear using monofilament non-absorbable material.
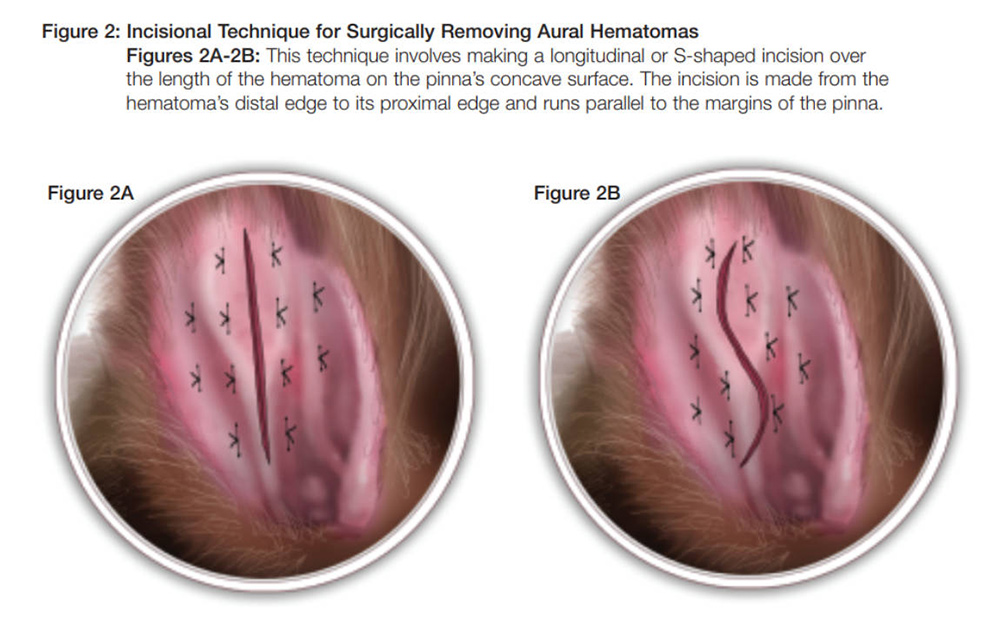
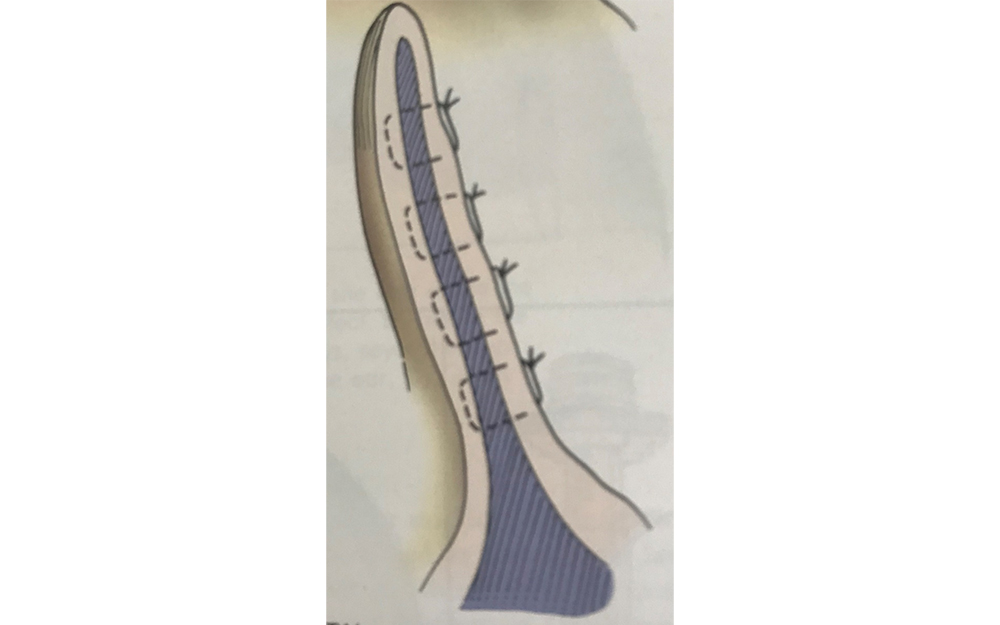
Figures 4/5 — Vertical sutures were placed either side of the surgical wound, which can be linear or 'S' shaped. C. Sutures were placed through the cartilage.
Post-operative care
After the surgery, a bandage was applied to the ear; an Elizabethan collar was also fitted to minimise the likelihood of further trauma.
Medication:
- Carprofen (NSAID) was given at 4 mg/kg once per day, by mouth, for 5 days
- Itraconazole at 5 mg/kg once per day, by mouth, for 4 weeks, to treat the Malassezia spp overgrowth
- Chlorpheniramine at 4mg twice per day, by mouth, for 7 days, to reduce irritation
- Both of Happy's ears were cleaned with an acetic acid-based ear cleaning solution (MalAcetic®) every 2 days. This solution contains 2% acetic acid and 2% boric acid, which has antibacterial and antifungal properties.
Seven days after surgery, the sutures were removed and Happy was closely monitored for any signs of reappearance of the haematoma.
Prognosis
The prognosis is usually good, as long as the underlying cause is identified and treated. In this case, treatment of the Malassezia pachydermatis infection may take some time to resolve. Long term ear cleaning and monitoring is likely to be required to prevent recurrence.
Discussion
An aural hematoma is formed by the collection of blood under the skin of patient’s ear flap (pinna). When a patient vigorously shakes their head or scratches their ear, trauma to the ear causes the blood vessels and capillaries in the pinna to rupture. When these vessels break, blood collects in the space between the skin and cartilage, creating a hematoma. This condition is usually unilateral, but it can be bilateral.
As discussed above, aural haematomas can occur secondary to pruritic or non-pruritic, mechanical trauma to the pinnae. Both primary and secondary causes of otitis externa can be involved, and it is important to identify these. Hypersensitivity reactions, especially atopic and food related causes, are the most common causes in dogs.
Diagnosis of aural haematoma should always involve an otoscopic examination, including an assessment of the integrity of the tympanic membrane. In addition, ear cytology should be performed.
Treatment options for aural hematoma can be divided into medical or surgical management, and what is suitable depends on the size and cause of the aural hematoma, and whether it recurs. Aural haematoma should be treated as soon as possible, otherwise the fluid can be re-absorbed and fibrosis can lead to contraction and thickening of the pinna, leaving the ear with a deformed cauliflower-like appearance. This can then be a predisposing factor to further ear problems in the future.
Medical management
Medical management can involve drainage and local or systemic drug treatment.
Drainage. This can usually be performed without sedation and is a good first step for treating simple aural haematomas. Aseptically prepare the medial aspect of the ear with a skin preparation solution (e.g. dilute chlorhexidine or povidone-iodine). Using a butterfly catheter (19 or 21G) and an appropriate sized syringe (a 10ml or 20ml should be appropriate, depending on the size of the haematoma), insert the needle into the medial side of the ear and withdraw as much fluid as possible. Try to minimise repeated puncture of the skin surface.
Local treatment. Intra-lesional steroid injections can be used after drainage:
- Methylprednisolone 10-40 mg, every 7 days, for 1-3 weeks
- Dexamethasone 0.2-0.4 mg (diluted in saline), every 24 hrs, for 1 to 5 days
Systemic treatment. Oral steroid administration may reduce the inflammation in the ear and prevent recurrence of the haematoma in cases where local treatment is not feasible (e.g. when the ear is too painful). 0.125mg-1mg/kg prednisolone every 24hrs for 10-14 days, tapering down after 7 days.
In cases where recurrence does occur, surgical management is warranted.
Surgical management
There are 4 principal surgical methods appropriate for the management of aural haematoma without specialist equipment.
- Linear incision. As described in the treatment method above, a linear or S-shaped incision is made on the medial aspect of the pinna and is kept open through the application of multiple, staggered, interrupted mattress sutures at a 90° angle to the incision.
- Cannula technique. The ear is drained as described in medical management. The trimmed teat of a large gauge cannula is inserted through the needle hole and sutured in place.
- Placement of a drain. The ear is drained as described in medical management. Incisions are made at the proximal and distal ends of the haematoma and a 1/4" fenestrated drain is fed through the length of the haematoma and sutured in place.
- Punch biopsy technique. The ear is drained as described in medical management. A dermal biopsy punch is used to make multiple openings across the medial aspect of the pinnae. Simple interrupted sutures can be placed along the skin of each punch hole.
Post-op management is important to ensure infection is not introduced to the pinna.
In this case, a linear surgical fixation, once chosen because it was a large hematoma. Assessing the literature, some texts suggest keeping the sutures in the ear for 2-3 weeks to ensure adequate tissue apposition.
Addressing the Underlying Cause: Malassezia pachydermatis
Malassezia pachydermatis is a commensal yeast. It is normally found in low numbers in the ear canal and mucocutaneous junctions of dogs. Malassezia pachydermatis has a characteristic round to oval or classical peanut shaped appearance with monopolar budding. Overgrowth of Malassezia spp is commonly seen as a secondary cause of otitis externa.
Treatment options will depend on what is available to you. Topical treatments containing antifungal drugs are often used once or twice daily to successfully to clear an infection. It is important to clean the ear with a proprietary ear cleanser first, to ensure that the medication will reach the skin surface.
If these products are not available, or if the patient is not compliant, systemic anti-fungal treatments can be used, such as:
- Ketoconazole (5-10mg/kg once or twice per day)
- Itraconazole (5-10mg/kg once per day)
- Fluconazole (5- 10mg/kg once per day), plus cephalexin
- Terbinafine (30mg/kg once per day), with or without cephalexin
Treatment should continue for 7-10 days after clinical resolution and a repeat cytology can confirm the reduction of yeast numbers. The prognosis depends on the primary cause of the overgrowth, but is generally good if this is addressed.
References
- Aural Hematoma | American College of Veterinary Surgeons - ACVS. Available at:
https://www.acvs.org/small-animal/aural-hematoma
[Accessed 26 February 2020.] - Hall, J., Weir S., and Ladlow, J. (2016). Treatment of Canine Aural Haematoma by UK Veterinarians. The Journal of Small Animal Practice 57(7) : 360–64. Available at:
https://doi.org/10.1111/jsap.12524 - Hewitt, J, Bakwa, J. Aural Hematoma and its treatment: A Review, The Canadian Veterinary Journal, 2020 March; 61(3): 313-315.
- Lahiani J. and Niebauer G. (2020). On the Nature of Canine Aural Haematoma and Its Treatment with Continuous Vacuum Drainage. The Journal of Small Animal Practice, 61(3) 195-200. Available at:
https://doi.org/10.1111/jsap.13107
[Accessed 13 August 2021] - Paul, P, and Spadafori, G. (2017). Veterinary Partne’. VIN.Com, 8 August 2017. Available at:
https://www.vin.com/doc/?id=8156779
[Accessed 13 August 2021]
About the author
Dr. Anupat Tanseree (aka “Dr. Earth”) has been working with WVS Thailand since June 2018 after his graduation at Chiang Mai University (May 2018). Since then has been proved to be an enthusiastic and proactive young vet, quickly learning and proficiently training up to WVS protocols.
© WVS Academy 2026 - All rights reserved.