We use cookies
We use cookies to ensure that we give you the best experience on our website. Would you like to accept all cookies for this site?
Samka, Traumatic Wound, Secondary Wound Closure
Introduction
Traumatic wounds are one of the most common injuries seen in shelter/charitable practices. The causes of injuries are usually varied, including: bite wounds, road traffic accidents, and intentional harm by people. In general, the wound treatment process involves reducing inflammation, controlling infection, debridement, bandaging and surgical reconstructive techniques, all of which encourage healing.
In this case report, Samka, a female community dog, was treated at the WVS Rescue and Rehabilitation Centre in Thailand. Samka presented with an extensive inguinal laceration wound with a bacterial infection that prolonged her treatment and challenged our veterinary team's skills.
Read about her case here.
History
A Thai, mixed-breed, female dog was brought to WVS Thailand after a road traffic accident. Her caretaker reported that Samka had an old injury affecting her right hind leg, from a previous traffic accident, but she could still use the leg well. Samka was found with a massive wound in her inguinal area with complete degloving of the region and some underlying muscle damage. The caretaker applied Gentian Violet to her wound before they brought Samka to us (Figure 1). Gentian violet is an antiseptic solution used to treat fungal infections and has weak antibacterial properties.


Figure 1 — Samka's wound on the first day that she presented to WVS Thailand
Signalment and Clinical Findings
Samka was a female, spayed, white-beige, mixed-breed dog, approximately 1 year old and weighing 14.2 kg.
Physical Examination
- Quiet, alert and responsive
- Body Temperature 38.4°C
- Behaviour: gentle, kind
- Cardiovascular System: normal heart sounds, pale pink mucous membranes, capillary refill time < 2 sec, strong femoral pulses
- Respiratory: normal lung sounds, clear TS
- Dermatology: normal hair coat, normal hydration. Large laceration wound in the right inguinal area, skin detachment 2.5 cm from midline down to stifle, and 2.5 cm below the patella. Right lateral attachment of the skin flap and deep pockets of dead space under the skin. Underlying musculature exposed.
- Body Condition Score: 3/5
- Musculoskeletal: old lesion from previous injury on right tibial crest, thickening and callus formation was found from palpation
- Neurological: all sensory and motor tests normal for damaged limb. No abnormalities detected elsewhere.
- Abdomen: normal
- Eyes, Ears, Nose, Throat: no ocular and nasal discharge
- Urogenital: normal
Differential Diagnosis
- Traumatic wound, skin laceration (Figure 2)

Figure 2 — Samka's wound when she was presented to WVS Thailand

Figure 3 — 3 days after daily cleaning; notice that the Gentian Violet is still staining the muscle and adipose tissue.
Initial Laboratory Findings
Blood Results
Complete Blood Count (CBC):Mild anaemia (Haematocrit 33%, reference range: 35-57%) , Lymphocytosis (Lymphocyte 34%, reference range: 8-21%).
Blood Chemistry:Elevated ALT (ALT 166 U/L, reference range: 10-108 U/L).
Radiographic Findings
The radiographs showed the chronic damage to the right stifle joint around the lateral trochlear ridge and lateral condyle of the femur and right tibial crest. Healed fractures of the left acetabulum joint were visible with callus formation already established (Figures 3 and 4).
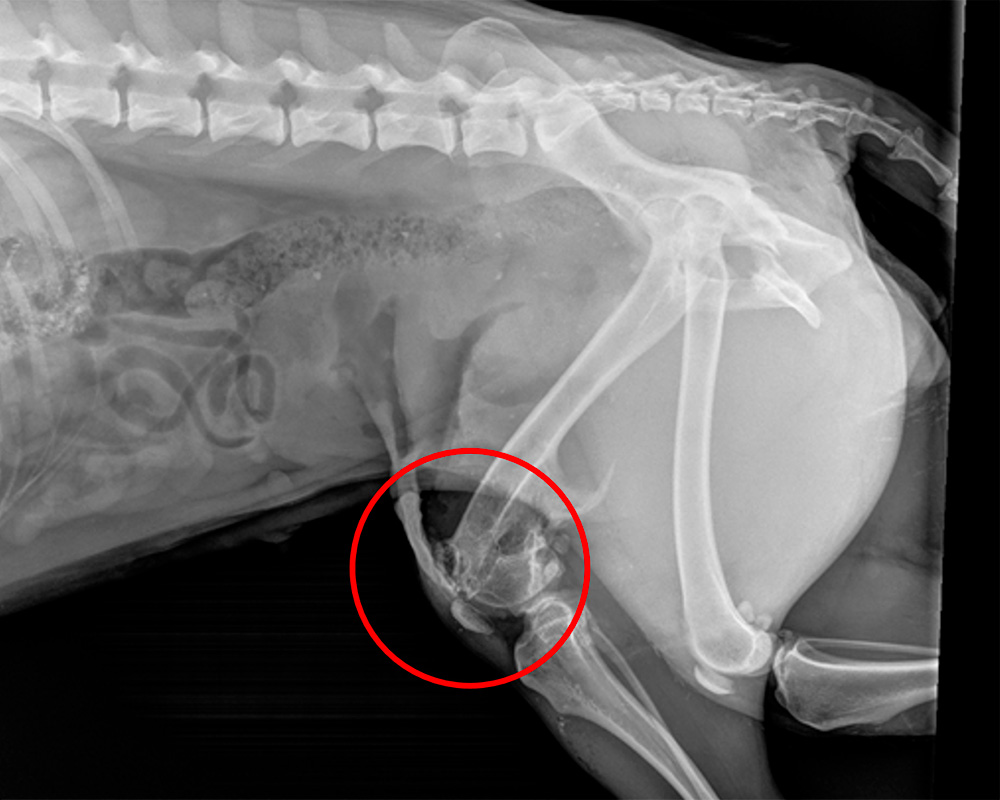
Figure 4 — Lateral radiograph of Samka's leg showing previous skeletal damage to her right stifle (circle).
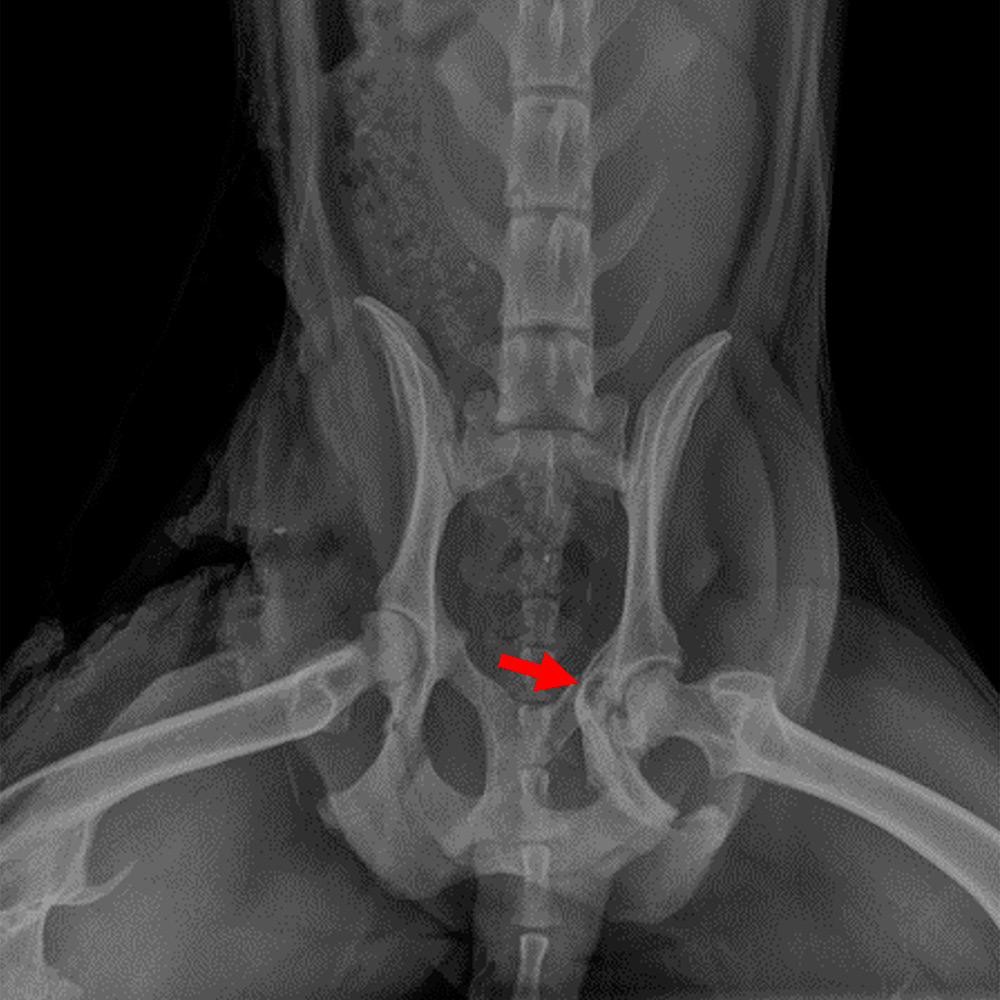
Figure 5 — Ventro-dorsal radiograph of Samka's pelvis showing left acetabular damage and callus formation (arrow) from a previous road traffic accident.
Initial Treatment
Samka was sedated to allow our vet team to properly cleanse the wound and remove all hair around it. Samka's caretakers applied Gentian violet to the wound before they came to us, so the purple stain on the wound made it difficult to differentiate between healthy and necrotic tissue, and to debride the wound effectively. The vet team scrubbed the area around the wound with chlorhexidine, then flushed the area with sterile saline and dressed the wound with a wet to dry bandage to remove gross contamination.
IV fluid therapy was given at maintenance to stabilise Samka and prevent shock. She was also given:
- Amoxycillin-clavulanic acid (amoxy-clav) 312.5mg by mouth twice per day for 14 days (recommended dose 12.4-25mg/kg by mouth q8-12hrs)
- Carprofen 50mg by mouth once per day for 5 days (recommended dose 4mg/kg q24hrs)
- Tramadol 50mg twice per day by mouth for 5 days (recommended dose 2-5mg/kg q12hrs)
The initial treatment was focused on stabilisation, administration of pain relief, and control of infection via oral medication and daily wound cleaning. This was vital to allow our vet team to accurately assess the area of necrotic tissue through removal of the Gentian Violet staining of the soft tissue structures. Samka was limping when she walked due to trauma, but the injured leg had full sensory and motor function and no neurological deficits.
Over the next few weeks, treatment focused on daily wound lavage and assessment of tissue by both debridement and using wet-to-dry bandaging to remove small debris and necrotic tissue. Considering a degree of tissue loss, the vet team determined that, at this stage, the skin would not be able to cover the wound, in particular because the site of the wound was a highly mobile area. Therefore, surgical reconstruction of the wound was not yet possible and the vet team opted for initial infection control and secondary wound closure.
A swab sample of the wound was collected for bacterial culture and sensitivity to focus the use of antimicrobials during this initial treatment phase.
Second Laboratory Findings
Bacterial Culture and Sensitivity
The result from the wound swab showed:
Culture Result: Proteus mirabilis.
Sensitive to: Amikacin, ceftriazone, ceftiazidime, cefotaxime, enrofloxacin, gentamycin.
Resistant to: amoxycillin, amoxycillin-clavulanic acid, cephalexin, cephazolin, clindamycin, metronidazole.
Treatment Plan
The laboratory results showed a multi-resistant bacterial infection which was only susceptible to Amikacin, 3rd generation cephalosporins, enrofloxacin and gentamycin. To control the infection, Enrofloxacin tablets (100mg by mouth once per day for 14 days, recommended dose 5mg/kg once per day) were prescribed orally for 2 weeks, and daily wound cleaning was continued (Figures 6 and 7).

Figure 6 — Samka's wound; note the granulation tissue forming. The wound started healing by secondary intention with epithelialisation and contraction medially and caudally.

Figure 7 — Cranial aspect of wound; note the skin from lateral side has rolled inward. Once the infection of the wound was controlled, this would need to be surgically corrected.
Once the enrofloxacin course was complete, the WVS Thailand vet team repeated a swab sample for bacterial culture and sensitivity.
Bacterial Culture and Sensitivity
The result from wound swab showed:
Culture Result: Psudomonas aeroginosa.
This bacteria was only susceptible to amikacin and 3rd generation cephalosporins.
Revised Treatment Plan
Based on the culture and sensitivity results, Samka was put on a regimen of intravenous ceftriaxone at 20mg/kg IV twice daily (recommended dose: 15-50mg/kg q12-24hrs) combined with continued wound cleaning.
Quarantine Measures
To prevent the spread of this multi-drug resistant bacteria to other patients in the Intensive Care Unit, quarantine measures were put in place. Samka was isolated in her kennel, caretakers had to wear an apron, gloves, different boots, and all of this personal protective equipment was disinfected before and after cleaning her kennel. Food bowls and cleaning equipment were used for only her kennel. Samka was treated at the end of the day after all other patients had been examined in the treatment room, and all surfaces and equipment used were thorough disinfected after her treatment.
After 2 weeks on the ceftriaxone antibiotic with wound cleaning for infection control and promote tissue healing (secondary intention wound healing), Samka's wound was getting much smaller due to epithelialization of skin. The wound had stopped producing significant amounts of exudate and the granulation tissue looked healthy. A final bacterial culture and sensitivity sample was taken to ensure that the infection was under control before surgical closure was possible.
Bacterial Culture and Sensitivity
The result from wound swab showed:
Culture Result: No growth of bacteria after 7 days.
Surgical Reconstruction
Surgical debridement and undermining was used to unfold the skin that had rolled inward and any remaining necrotic or devitalise tissue was removed (Figure 8).
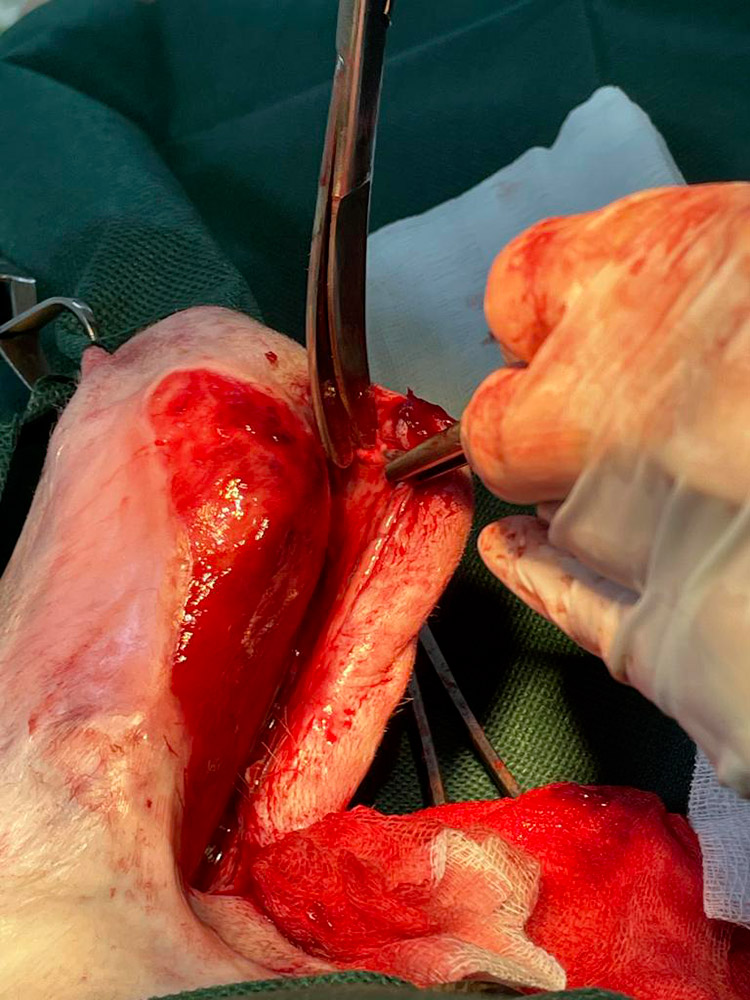
Figure 8 — Undermining of the skin
The loose skin flap was then pulled across the wound to measure how much would need to be trimmed for accurate skin apposition. Also, the skin around all the edges of the wound was undermined partially resecting around the granulation bed (Figures 9 and 10).
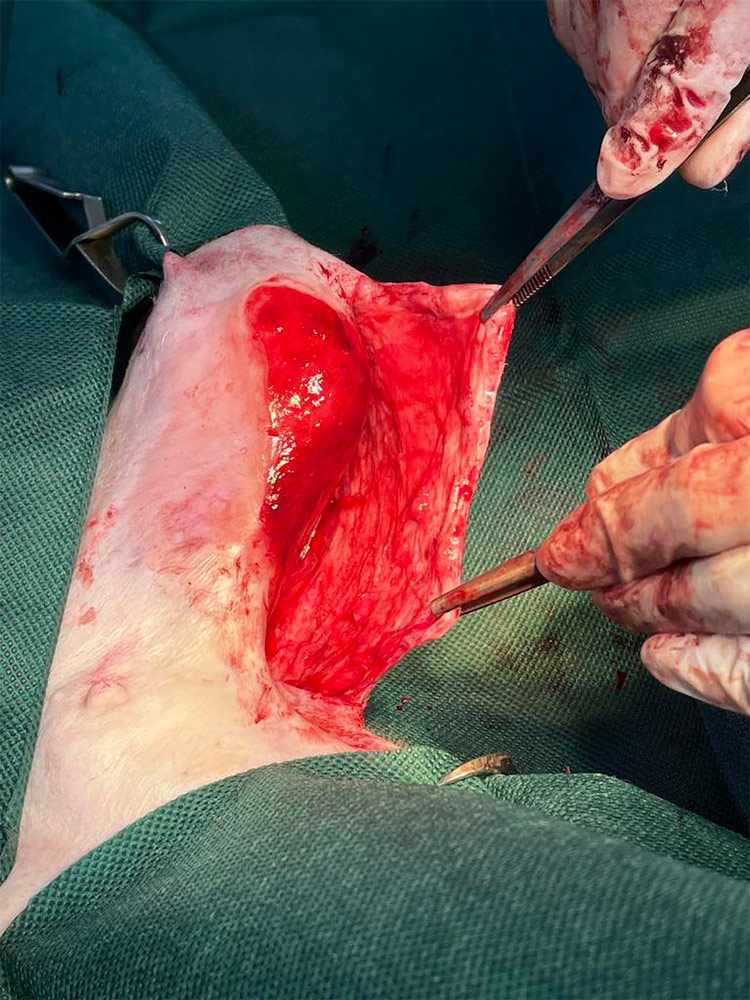
Figure 9 — Skin flap is manoeuvred over the wound defect.
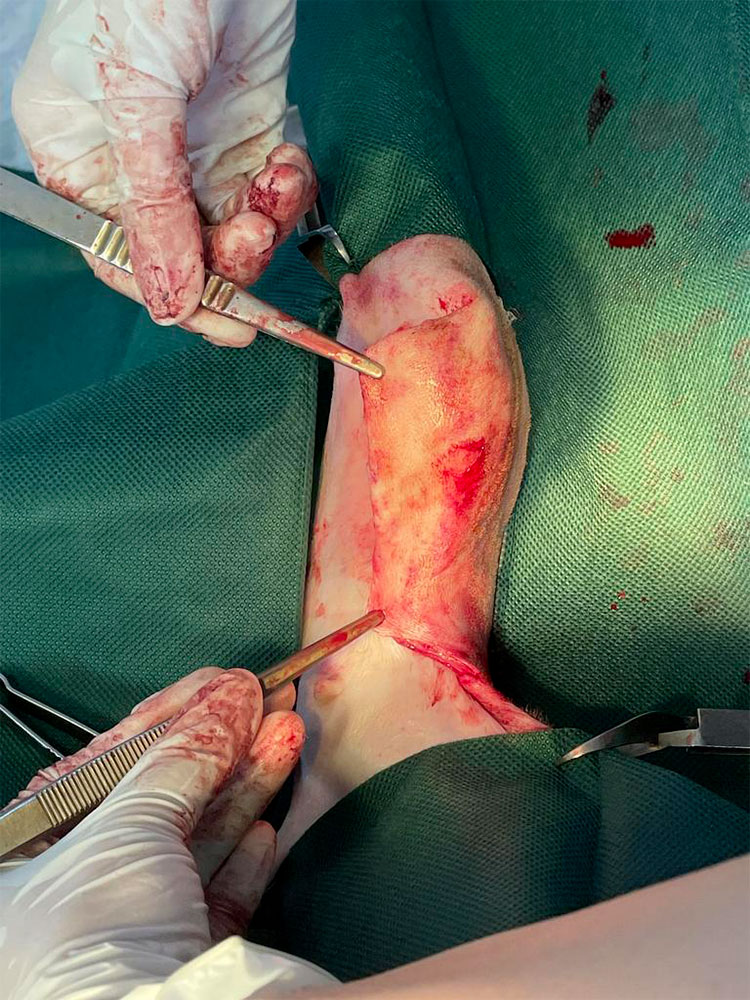
Figure 10 — Skin flap adjusted to cover the skin defect, reading for suturing.
Walking sutures were placed using monocryl 2/0 to relieve tension before the skin sutures were placed.
Skin closure was achieved using Supramid 2/0 in a simple interrupted pattern to appose the skin flap edges. A small section of granulation tissue at the medial stifle was not able to be covered by the skin flap (Figure 11).

Figure 11 — The skin edges are apposed along the majority of the wound edges using simple interrupted sutures.
Prognosis
Good – with the infection under control before surgery and almost complete wound edge apposition, the biggest risk was suture breakdown. The WVS surgeon reduced this likelihood by using tension relieving sutures.
Outcome
The wound healed properly without complications. There was no wound dehiscence, and the stitches were removed 7 days after the surgery. It took a couple more weeks for Samka's wound to be fully healed because the wound location was on a very mobile area and there was skin contraction from secondary intention healing (Figure 11). The vet team added in physical therapy and laser therapy for mobility and pain management during her recovery.

Figure 12 — Samka's wound after her treatment was complete.
Discussion
Determining appropriate wound management
Wound management depends on the degree of contamination, the time since the wound occurred, and the nature of the wound (location, size, depth, structures involved). There are 4 main types of wound healing:
Primary wound closure — surgical closure within the 'golden period' for wound closure (6-8 hours).
Delayed primary wound closure — first ensuring that the wound is free of infection and closing the wound surgically before granulation tissue has appeared. Usually after 3-5 days of bandaging and debridement.
Secondary closure — allowing a granulation tissue bed to form before surgically closing the wound, often using a flap or a graft if there is a tissue deficit.
Second intention healing — allowing the wound to close through contraction and epithelisation.
If wounds are closed when there is contamination, necrotic tissue, excessive tension, or dead space, they are at a higher risk of breaking down (dehiscence).
Factors that affect the decision to close wounds include the following (taken from Fossum et al, Small Animal Surgery):
- Amount of time that has elapsed since injury. Wounds older than 6 to 8 hours are initially treated with bandages.
- Degree of contamination. Obviously contaminated wounds should be thoroughly cleansed and initially treated with bandages.
- Amount of tissue damage. Wounds with substantial tissue damage have reduced host defences and are more likely to become infected; therefore, they initially should be treated with bandages.
- Completeness of debridement. Wounds should remain open if the initial debridement was conservative and if further debridement is necessary.
- Status of wound's blood supply. A wound with questionable blood supply should be observed until the extent of non-viable tissue is determined.
- The animal's health. Animals unable to tolerate prolonged anaesthesia are best treated with bandages until their health improves.
- Extent of tension or dead space. If excessive tension or dead space is present, wound should be bandaged to prevent dehiscence, fluid accumulation, infection and delayed wound healing.
- Location of the wound. Large wounds in some areas (e.g. limbs) are not amenable to closure.
This case
In this case, Samka was involved in a road traffic accident, causing a massive laceration in her inguinal region. The accident had occurred longer than 6-8 hours ago and the wound was badly contaminated, so primary closure was not an option. The initial treatment provided was to stabilise Samka and reduce the degree of contamination through wound cleansing and bandaging, as well as wound debridement.
Unfortunately, while the wound was forming a granulation tissue bed, antimicrobial resistant bacteria were found by bacterial culture, which showed multi-resistance to several first generation antibiotics. Consequently, the use of enrofloxacin and then a 3rd generation cephalosporin in this case was necessary.
The quarantine measures put in place after the discovery of the multi-drug resistant bacteria were crucially important to avoid spreading of the bacteria to other animals in the intensive care unit. Unfortunately, WVS Thailand doesn't yet have a dedicated quarantine unit, and so maximum precautions needed to be taken to prevent vector spread of the bacteria. The clinic vet conducted Samka's treatment at the end of each day and all surfaces and equipment used were thoroughly cleaned after her treatment. Caretakers used separate cleaning equipment e.g. mops and brushes, and they also wore an apron, gloves, boots, and disinfected them before and after entering Samka's kennel.
The use of bacterial culture and sensitivity was incredibly important to the progression of this case. Establishing the type of bacteria and the specific drugs which were effective against them aided the wound healing significantly.
Once the infection was controlled, surgical reconstruction of wound was scheduled and performed. Fortunately, there was sufficient skin to cover the entirety of the wound, once there had been some contraction and epithelisation. If this hadn't been the case, there would have been the option of a skin graft or a skin flap, although in this particularly mobile area of the leg, both options would have required substantial surgical skill.
If there were even less resources available or there was more significant damage to the skeletal or nervous systems of the leg, the option to amputate would have been a reasonable one. Amputation should always be considered if the time and resources (in a resource-scarce setting) and animal suffering which would be involved in the case is likely to be high.
References
- Theresa W. Fossum. Small animal surgery. Third edition (pp.409 to 413). St. Louis, Mosby Elsevier

About the author
Dr Santiparp Kornakaew (aka Poppy) is the Senior Thai Vet at WVS Thailand; has been working with WVS since 2015, has attended dozens of Rescue Cases and has mentored over 200 students, Thai and International, as part of our Training Program.
© WVS Academy 2026 - All rights reserved.